Startup Healthcare Benefits Explained: Deep Dive
.png)
Once you’ve raised some seed money and gotten yourself on payroll, the next step is to secure healthcare benefits for you, your co-founder, and any new potential hires.
But how do you navigate the U.S. healthcare insurance world and choose the right healthcare benefits for your startup?
What are healthcare benefits?
Healthcare benefits include medical, dental, and vision insurance coverage, so you can visit the doctor and get the care you need – whether it’s preventative care, prescription meds, or surgery. You may have enjoyed private healthcare benefits offered by your large employer, your parents’ health insurance, or, if outside the US, through government-sponsored national health insurance programs.
If you or any of your employees become ill or have an accident, you’ll want to ensure you have healthcare coverage in place. Why? Because healthcare in the US is expensive. Hospitalization and surgeries can cost anywhere between $4000 and $200,000 without insurance, according to the 2023 Milliman Health Cost Guidelines. You and your new employees don’t want to take this risk.
In the US, healthcare coverage is not free, and healthcare insurance is usually offered as a “benefit” by employers (yes, that’s you now that you’ve founded a company). In fact, U.S. employers with 50 or more employees are required by law to provide healthcare benefits.
However, even a small, early-stage startup with just a few employees will want to offer healthcare benefits as a key part of its overall compensation package to attract and retain the talent necessary for success.
Guiding startups through the benefits process
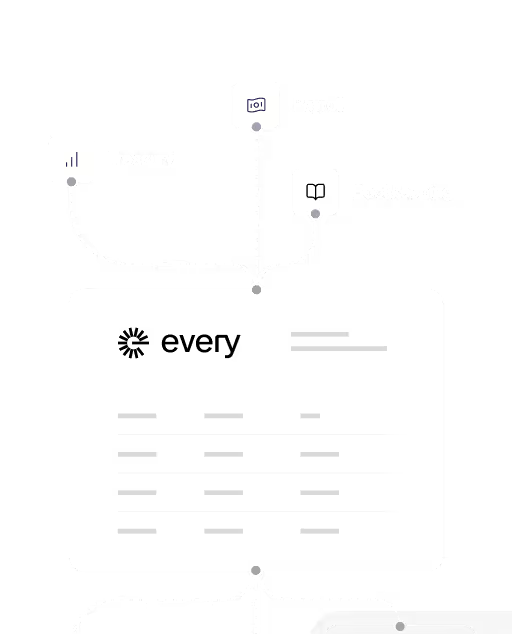
At Every–an all-in-one platform that includes HR, Payroll, Compliance, and Benefits–we help our startup customers select the right healthcare benefits for their budget and unique situation.
We meet with our founders at the beginning to determine their needs, explain how healthcare benefits work for startups, and set expectations. Many founders may be used to working for large employers that cover their healthcare benefits.
But shopping for small group health insurance is a different experience. Small group health insurance in the US is a highly regulated industry with premiums set at the state level.
At Every, we guide our founders through the process step by step, cutting through the noise and surfacing health plans that are just right for your startup and workforce demographics. For example, you might be a young founder trying to save money while also utilizing benefits as part of your talent attraction strategy, or you might be a startup with employees across multiple states.
Having guided many founders through the benefits process, here are some key tips to keep in mind when selecting healthcare benefits for your startup.
6 Tips for choosing healthcare benefits for your startup
1. Think beyond yourself and into the future
When many first-time founders shop for benefits, they naturally think only about their own needs. That might make sense since you, as the founder, are the first employee, but approaching benefits in this “founder-first” way is shortsighted. The plan you choose should also work for the employees you’re bringing on in the next 6–12 months.
- Young founders often underestimate the importance of strong coverage, but family-oriented hires will care deeply about richer plans.
- Seasoned founders often default to premium plans, but those can quickly become unsustainable as the team grows.
Instead of choosing healthcare benefits for yourself, ask: Will this plan attract the kind of talent I want, and can I afford it over time?
If you have the resources and the runway, founders should always think long-term about their healthcare benefits strategy. As you begin hiring, benefits are often key recruiting tools for attracting talent. Therefore, you’ll need to develop a range of benefit options that cater to your current and future needs. At the same time, if you have limited resources, it’s okay to offer basic medical coverage and scale as you grow.
2. Consider your startup’s group eligibility when choosing a plan
Often, founders want the healthcare insurance they’ve been using while employed at a large company. However, this is not always possible. Healthcare insurance carriers have specific eligibility requirements that determine which companies are eligible for coverage and which are not.
You’ll also want to consider whether you are a remote-first company and plan to hire across state lines or even internationally. Moreover, your HQ location matters, as that’s where your healthcare carrier will underwrite your plan and set your premiums. And some states, like New York, are more expensive than others.
At Every, we help startup founders identify the right insurance carriers based on group eligibility requirements.
When shopping for healthcare insurance carriers, here are some of the different group qualification rules carriers might have:
- Some carriers require newly established companies to be in business for at least six weeks and demonstrate at least two weeks of payroll.
- Most carriers require either (a) founders plus at least one W-2 employee or (b) two or more owners on payroll. Solo founders and owners who are married to each other generally do not qualify.
- Some carriers won’t underwrite your startup if employees are too dispersed. (For example, if you don’t have 51% employees in one state or your two founders are in different states).
- An HMO plan works if all your employees are in one state, but if you hire an employee in another state, it won’t cover them.
- PPOs generally offer more flexibility for distributed teams than HMOs.
- Your insurance rates are based on your HQ location and where you have the most employees. But if you hire more employees in another state, that may change where your insurance is underwritten and, subsequently, your rates.
- US small group health insurance policies do not cover international employees. However, at Every, we help startups cover international employee health benefits through a third-party Employer of Record (EOR).
Participation also matters to carriers.
In addition to the above requirements, carriers also require a certain percentage of your eligible employees to enroll in the plan. This is called a participation requirement.
Carriers establish participation rules to ensure the group risk pool isn’t dominated by a few sick employees who select coverage.
- Typical participation rule: At least 50%–65% of eligible employees must enroll in your health plan. Some carriers may allow as low as 25% participation if you have five or more employees and qualify for a relaxed participation period.
- Who counts as “eligible”? Usually, all full-time W-2 employees who work at least 30+ hours per week. Owners can count if they are on payroll.
- Who doesn’t count against you? Employees who decline coverage through a valid waiver (e.g., they already have insurance through a spouse, parent, or another job) are usually excluded from the participation calculation.
So, for example, if you have five full-time employees, at least three must enroll. If one opts out because they’re covered under a spouse’s plan, then only four count as eligible, and two (50%) must enroll to meet the participation requirement.
Founders planning to hire slowly should think about participation early — if only one or two employees want coverage, you may not meet the requirement.
Plan ahead
Plan ahead because you can’t switch providers midstream. You can only make changes to your health plan insurance once a year.
That’s why at Every, we consider your startup’s long-term hiring strategy when recommending the right health plan. For example, suppose founders are weighing HMO versus PPO networks but plan to scale as a remote-first company down the road. In that case, we’ll recommend a PPO option from a carrier that offers strong coverage across multiple states.
3. Think of benefits as an evolving strategy
The good news is that you don’t have to look that far into the future. Every year, you can renew and revise the benefit plan that works for your startup.
However, remember that it’s usually challenging to claw back benefits once you've offered them, so start small and expand your benefits offering as you grow. Employees will see the initial contribution amount as their anchor point, and many will be disappointed if support is rolled back.
As you consider your offerings, think of benefits as an evolving strategy. Here are a few things to think about:
Understand company contribution basics
- Covering 90%–100% of employee premiums signals that you value your team’s health and helps position benefits as a recruiting tool.
- Dependent coverage (spouses/children) is optional. Carriers don’t require it, and employer contributions can range from 0% to 50% (competitive) to 80% (most competitive), and very rarely 100%. Offering dependent coverage can make you more attractive to experienced hires with families.
- All carriers in California require a minimum employer contribution of at least 50% for the employee; however, you are not required to contribute toward dependents.
Typical contributions by startup stage
Based on your startup stage, you’ll want to scale and improve your benefit contribution level as you grow.

Offer a range of health plan options
- Offer a range of health plan options for your employees to choose their level of comfort in terms of monthly premiums and out-of-pocket costs, e.g., Bronze, Silver, Gold, and Platinum options.
- For example, an older employee might opt for the Platinum level, which comes with a higher monthly premium but lower out-of-pocket costs.
- In contrast, a younger employee might prefer the Bronze level, characterized by a lower monthly premium and higher out-of-pocket costs should they become ill.
- Leverage your company's contribution strategy to effectively incentivize employees to choose the health plan that best suits their needs. This saves the company money while offering employees choice and options. For example, consider offering a Silver plan as a base, but adding upgrade options for employees to pay the difference.
Add dental and vision plans
- Finally, consider adding dental and vision — they’re inexpensive but highly valued.
- Choose plans based on the maximum benefit. Typically, a maximum dental benefit of $1,500 to $2,000 works for most people.
- Always ensure that the dental plan you choose covers 100% of preventive care.
- Vision usually includes an annual exam and a small allowance for frames and contact lenses.
Reassess your benefits annually
- Finally, revisit your benefits annually and continually enhance them as your company grows.
- An annual survey on how employees use their benefits can inform whether your base plan needs to be adjusted.
- Reassess costs, provider access, and other relevant factors annually.
- Founders can expect a rate lock for 12 months, but should expect annual increases of 5-15% for renewals of the same plan.
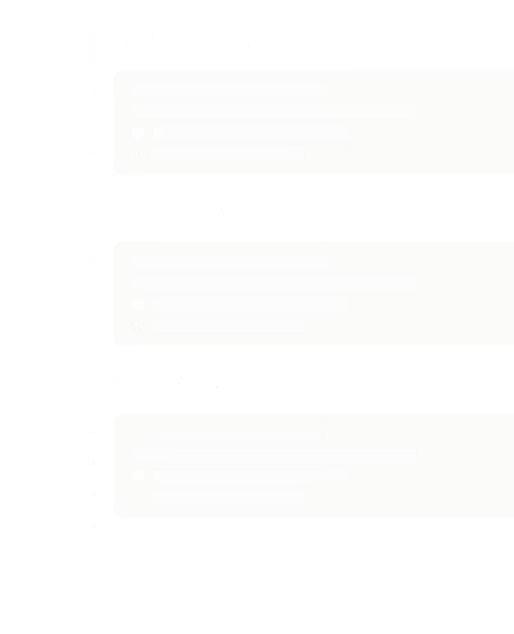
4. Understand the timeline (and set expectations)
Most founders assume benefits can go live immediately as soon as Payroll goes live on the Every platform, but this is an unrealistic expectation. The benefits approval process usually takes one month after Payroll goes live.
This is mainly because carriers will require a two-week payroll journal prior to underwriting healthcare insurance for an employee.
So, for example, if your group applies for benefits in mid-August, you're application won't be considered complete until your 2-week payroll journal is submitted at the end of August.
The carrier will likely approve your health insurance the second or third week of September, and we can then backdate the effective coverage date to September 1.
Here are a few things to consider when it comes to the timeline:
- Expect backdating: Carriers often approve coverage weeks after the effective date. (This is especially true if you start the application with less than a month before the desired effective date.)
- Don’t schedule unnecessary doctor’s appointments before approval. However, emergency claims can usually be submitted retroactively.
- Set expectations with your team early to avoid confusion.
5. Get help navigating the application and underwriting process
After you submit your healthcare insurance application to the carriers, they’ll likely ask for more information or further explanation. At Every, we help quarterback the paperwork and carrier communication to save founders weeks of back-and-forth and ensure you don’t miss deadlines.
These are usually the typical documents you’ll need to submit with your application:
- Your startup’s federal tax return for proof of ownership.
- Foreign qualification in your HQ state, as that’s where your insurance will be underwritten.
- Payroll requirements – you need W-2 employees to qualify; a founder can be a W-2 employee. For example, if your startup has two founders, both of you need to be on Payroll and classified as W-2 employees to qualify for small group insurance coverage.
- Finally, you’ll need to submit proof with a 2-week Payroll Journal.
Because we handle most of the legwork for our startup customers and ensure the process runs smoothly, it typically takes only a few hours of founder time to set up benefits with Every.
6. ICHRA as a fallback
Finally, most carriers don’t cover solo founders with zero employees or founders/employees who aren’t on payroll. This is because they don’t meet the minimum group size requirements for a small group health insurance plan.
In this case, we recommend an Individual Coverage Health Reimbursement Arrangement (ICHRA). This is an excellent option if you’re at the very early pre-seed stage of your startup.
- ICHRA is a flexible alternative for founders who don’t yet qualify for group plans.
- At Every, we offer ICHRA through our partner, Thatch.ai.
- Startups can cancel their ICHRA plan and apply for a group plan when they become eligible.
Benefits as a recruiting tool
Healthcare benefits are not a checkbox exercise. Benefits are a strategic investment that offers a critical tool for talent recruitment for your startup. By thinking long-term, planning for distributed teams, and setting realistic expectations, you can structure your benefits to put your startup in a stronger position to attract great talent without breaking the bank.
Partner with Every, and we’ll help you navigate the small group insurance landscape to identify the best healthcare benefits for your startup. Request a demo.